Epidural Anesthesia Needle
Epidural needles are indispensable tools in the field of anesthesiology and pain management. Used primarily during childbirth and various surgical procedures, these needles play a crucial role in providing localized Epidural Anesthesia Needle and pain relief. This comprehensive guide aims to delve into the intricacies of epidural needles, from their mechanism of action to the procedure of insertion and associated considerations.
Understanding Epidural Needles
Epidural needles are specialized medical instruments designed to deliver medication directly into the epidural space of the spine. This space surrounds the dura mater, a protective membrane covering the spinal cord and nerve roots. By accessing the epidural needle, epidural needles enable precise administration of local anesthetics, opioids, or a combination of both, providing effective pain relief or anesthesia.
Applications of Epidural Needles
Epidural needles find extensive use in clinical settings, with two primary applications:
Labor and Delivery: Epidural analgesia is commonly administered during childbirth to alleviate labor pains. The placement of an epidural needle allows for continuous infusion of local anesthetics, providing mothers with pain relief while maintaining mobility and sensation in the lower body.
Surgical Anesthesia:
Epidural anesthesia: Epidural is also utilized in various surgical procedures, including cesarean sections, orthopedic surgeries, and thoracic surgeries. By blocking nerve impulses from specific regions of the body, epidural needles facilitate pain-free surgery while allowing patients to remain awake and responsive.
Patient Positioning: The patient is positioned either sitting up and leaning forward or lying on their side with their back curved to facilitate needle insertion.
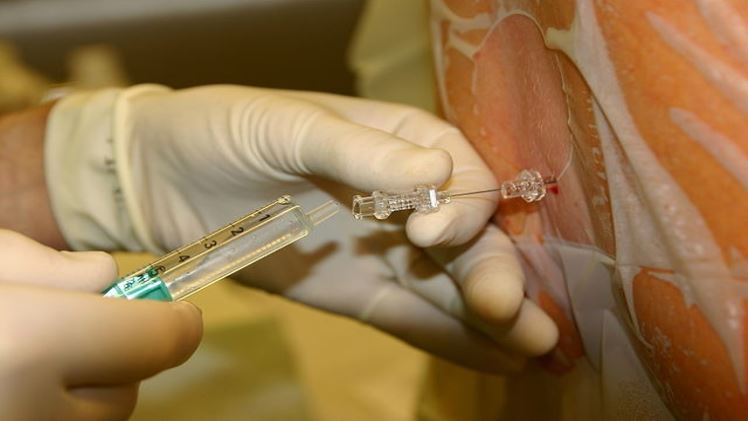
Sterilization and Local Anesthesia: The insertion site on the lower back is cleaned and sterilized, followed by the administration of local anesthetic to numb the area.
Needle Insertion and Medication Administration: The epidural needle is carefully inserted into the epidural space under fluoroscopic or ultrasound guidance. Once in position, medication, typically a combination of local anesthetic and opioid, is injected to provide pain relief or anesthesia.
Optional Catheter Placement: In some cases, a catheter may be threaded through the epidural needle into the epidural space to allow for continuous medication infusion.
Considerations and Risks: While epidural needles are generally safe, there are potential risks and considerations to be aware of:
Risks: Possible complications include headache, nerve damage, infection, and bleeding. Healthcare providers carefully assess each patient’s medical history and monitor for adverse reactions during and after the procedure.
Patient Communication: Effective communication between patients and healthcare providers is essential to address any concerns and ensure comfort and safety throughout the procedure.
Monitoring and Post-Procedure Care: Continuous monitoring of vital signs and neurological function is crucial post-procedure to detect any signs of complications. Patients receive instructions for post-procedure care, including activity restrictions and pain management.
Epidural needles are vital tools in pain management and anesthesia, offering patients relief during childbirth and surgical procedures. Understanding their mechanism of action, applications, procedure, and associated considerations epidural anesthesia needle empowers both healthcare professionals and patients to make informed decisions and optimize treatment outcomes. Effective communication, careful monitoring, and adherence to safety protocols are essential for successful epidural needle placement and patient care.
Needle Epidural
Epidural needles are integral components of pain management and anesthesia, providing targeted relief during labor, delivery, and surgical interventions. Their versatility extends to various medical contexts, including chronic pain management and palliative care. In obstetrics, epidural analgesia offers mothers significant pain relief during labor while allowing them to actively participate in the birthing process.
This method is especially beneficial for prolonged or difficult labors, reducing stress and enhancing the overall birthing experience. Moreover, epidural anesthesia needle plays a pivotal role in surgical settings, facilitating complex procedures with minimal discomfort for patients. Its ability to selectively block nerve impulses makes it a preferred choice for surgeries involving the lower abdomen, pelvis, or lower extremities.
Additionally, epidural needles are increasingly utilized in the management of chronic pain conditions, such as back pain and neuropathic pain, offering long-lasting relief and improving patients’ quality of life. The precise delivery of medication to the epidural space allows for targeted pain relief without the needle epidural systemic side effects associated with oral medications. Furthermore, in palliative care, epidural analgesia provides terminally ill patients with comfort and dignity, allowing them to spend their final days with reduced pain and enhanced mobility.
The procedure for placing an epidural needle requires meticulous attention to detail and adherence to strict safety protocols. Healthcare providers undergo extensive training to master the technique and minimize the risk of complications. Patient assessment plays a crucial role in determining the suitability for epidural analgesia or anesthesia, considering factors such as medical history, allergies, and previous experiences with anesthesia.
During the procedure, continuous monitoring of vital signs and neurological function ensures early detection of any adverse reactions, allowing for prompt intervention. Moreover, patient education is paramount to alleviate anxiety and promote active participation in decision-making. Clear communication regarding the procedure, potential risks, and expected outcomes empowers patients to make informed choices and feel confident in their care team’s expertise.
Despite the benefits of epidural needles, it is essential to acknowledge the associated risks and limitations. While rare, complications such as post-dural puncture headache, nerve injury, and infection can occur and require prompt management. Healthcare providers meticulously assess each patient’s risk profile and employ strategies to minimize adverse outcomes.
Patient comfort and satisfaction are prioritized throughout the process, with measures such as pre-procedure relaxation techniques and post-procedure pain management protocols implemented to enhance the overall experience. Collaborative multidisciplinary care involving anesthesiologists, obstetricians, nurses, and other allied healthcare professionals ensures comprehensive support for patients undergoing epidural procedures, promoting optimal outcomes and patient safety.